In this blog you will get more information about dry eye remedy and details on how to treat meibomian gland dysfunction with the latest methods.
Most of this information is gathered from The Dry Eye Handbook, which provides very effective dry eye treatment guides.
Most of this information is gathered from The Dry Eye Handbook, which provides very effective dry eye treatment guides.
HOW TO TREAT MEIBOMIAN GLAND DYSFUNCTION
Meibomian gland dysfunction is disorder that leads to dry eye syndrome. It is sometimes termed MGD, meibomitis, and posterior blepharitis. The disease is multifaceted, but it usually involves infection in the meibomian glands of the eyelid, which extrude the lipids (meibome) that are needed for the outer layer of the tear film. The swelling may arise because of a clog on the gland outlet at the eyelid margin.
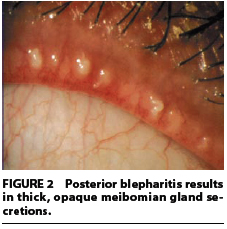
The clog, in turn, may be result from an eyelid enlargement from allergies or anterior blepharitis (in the front of the eyelid). Meibomian gland dysfunction may also be due to hormonal secretions, or dietary habits that influence the viscosity of the lipid secretions. Sometimes, the secretions may appear sandy and gluey, or even toothpaste-like; at other times, a firm fatty lump may form at the opening, sealing it. Another variation of MGD may involve copious extrusions of fatty substances irritating the eyes, although no jamming of the glands occurs.
The net result is that due to the disease, the lipid secretions of the gland become abnormal. There may be an excess of or a lack of oil; the oil may be too thick or too light. The consequence is that there is little stability in the tear film and evaporation happens at abnormal rates.
Meibomian Gland Symptoms
The manifestations of the disorder typically look like those associated with dry eye in general: burning sensation in the eye, grittiness, foreign body sensation, a mild fear of light because of high sensitivity, and crusting along the lid margins. The lid margins look engorged and inflamed and the inner rim of the eyelid may be hollowed as a result of scarring.
MGD often arises together with inadequacy of aqueous tears. When this happens, in all probability you will have specially severe dry eye manifestations. Approximately 60 per cent of Sjögren's syndrome patients (who exhibit aqueous tear inadequacy) have been observed to also suffer from MGD. Other skin diseases like rosacea and seborrhoea - which often result in blepharitis - are also associated with MGD. These linked disorders should also be addressed during the treatment of meibomitis.
The probability of developing meibomian gland dysfunction is noted to increase with age. It may be that the meibomian glands slowly degenerate in their functioning, or that age-related alterations in the eyelids may lead to abnormal blink mechanisms. What has been noted is that normal eyelids in seniors exhibit many of the changes in structure and form noticed in MGD.
MGD is also a result of long-term contact lens use. Contact lenses speed up the tear evaporation rate. Rapid evaporation can induce contact lens intolerance and worsen the intolerance in people whose tear films are already compromised to begin with. Similarly, meibomitis is also generally noticed in patients with giant papillary conjunctivitis (GPC) and chalazion (plural, chalazia; a lump that remains after a sty on the eyelid heals).
Meibomian Gland Treatment
MGD, being a rather intricate dysfunction, has many possible causes. In any person, the disease may begin from one or more of these causes. Your physician will have to consider them as the treatment program progresses.
The first order of business in treatment is to control inflammation on the eye surface, in order to dampen the damage from bacterial activity on the eyelid rim, enhance lipid function, and provide relief from the corollary dry eye symptoms.
Topical steroids may be recommended to manage inflammation, although this is not immediately resorted to because of the high risk of side effects. But newer compounds, such as loteprednol, are less risky and are moderately effective at reducing inflammation. Specially formulated topical cyclosporine, such as cyclosporine emulsion in a castor oil base, has also been used successfully to treat eye surface inflammation.
Essential fatty acids, particularly omega-3 fatty acids, have been mentioned in many informal reports with the potency to decrease dry eye symptoms, probably because of their well-established anti-inflammatory properties. Their anti-inflammatory action has also been observed to benefit meibomian gland disease.
Lid scrubs can be quite helpful. Cleaning the eyelid margin helps dislodge bacteria and their toxins, as well as clears meibomian gland ducts. Overzealous cleansing can lead to inflammation, however, and should be avoided. Punctal plugs, artificial tears (without preservatives), and tear stimulants also provide relief.
MEIBOMIAN GLAND PROBING TREATMENT
Dry eye syndrome gives rise to a burning sensation in the eye with a lot of itching, grittiness, redness and puffiness, increased sensitivity to light, blurry vision, and other discomforts. It arises from a variety of roots such as infections, other dysfunctions in the immune system, increased contact lens use, gland dysfunctions, and even medications taken for other diseases. Whatever the source of the ailment, the basic effect is that there is less volume of tears produced and tear quality gets so substandard that it evaporates more quickly.
Perhaps as many as three out of four dry eye patients also suffer from meibomian gland dysfunction (MGD) dry eye patients. The meibomian glands produce all the oily secretions that that constitute the lipid layer of the tear film, making the tears stable and less vulnerable to evaporation. There are about 30-40 meibomian glands in the upper lid and 20-25 in the lower lid. The lipid production in these glands may drop abnormally as a result of bacterial infections of the eyelids (such as blepharitis), skin conditions (such as rosacea), or side effects of drugs.
MGD is a bewildering disease. There are two basic manifestations, meibomian seborrhoea and meibomitis. Meibomian seborrhoea is manifested in overactivity in lipid secretions or easily expressed secretions. In this condition, the secretions are produced in amounts more than necessary, and it may consist of substances that can be damaging to the cornea. Meibomitis is manifested as a swelling of the glands due to bacterial infection, usually staphylococcus, and may be compounded with seborrhoea or rosacea. In this condition, the secretions are too sticky and can produce an obstruction in the orifices of the meibomian glands. Meibomitis quickly turns into swelling and inflammation along with long-lasting eyelid tenderness. Meibomitis is also referred to as obstructive MGD.
Meibomitis can pose a formidable challenge. The traditional approach is to apply warm compresses followed by gland expression. A recently developed technique for cleaning the meibomian glands holds some promise. The underlying principle involved is to use a probe attached to a very small, hollow and ductile stainless steel tube (called cannula) to get a feel of the canals stretching out from the meibomian glands. Probes of a variety of diameters are used, depending on the size of the ducts.
The probe/cannula is introduced into a meibomian channel until it encounters the blockage indicative of obstructive MGD. Once there, the physician may use the probe/cannula to suck the secretions or to apply some anaesthesia and try to eliminate the obstruction. Sometimes only those ducts with plugs are cleared. Sometimes all canals are cleaned as a preventative measure. The treatment can take between 5 and 30 minutes to complete, depending on the extent of obstructions and the patient's comfort.
After the obstructed canals are decongested, the meibomian secretions flow more normally and the associated dry eye symptoms may subsequently disappear. Eyelid massage and gland expression are well-suited methods for clearing plugs in the meibomian ducts. But for the more unyielding obstructions, MGD probing more effective technique.
MGD probing can provide relief for up to 18 months. After the procedure is done, you are encouraged to continue eyelid scrubs and heat compresses. These will prevent the formation of more gland obstructions.
MEIBOMIAN GLAND AND HOT COMPRESS TREATMENT
When the glands involved in tear production cannot produce the required volume of tears or tears of the proper quality, you will experience dry eye symptoms. The condition results in ceaseless irritation of the eyes, especially on waking up after a night's sleep. It causes grittiness, burning, itching, foreign body lodged in the eye, and assorted similar discomforts. Dry eye left untreated can result in damage of the cornea and, at worst, loss of vision.
Dry eye is very closely linked with meibomian gland dysfunction (MGD).. MGD accounts for up to a quarter of dry eye patients. Dysfunction in the meibomian glands may not retain the heat for as long as you may want. Many people have found rice baggies more appropriate. A rice baggy consists simply of some dry uncooked rice put in a cotton sachet big enough to completely cover the eyelid. Put the sachet in a microwave and heat until a suitable temperature is reached. You can experiment with different amounts of rice and heating times until you perfect the process. Place the heated sachet over the closed eyelid for up to 20 minutes. Rice baggies can keep heat much better than washcloths and distribute the heat more evenly because of their weight.
You can also heat a potato in a microwave but the weight (and therefore the heat) distribution is not as uniform as rice baggies. A freshly boiled egg wrapped in washcloth may also be used. Boiled eggs emit warmth for a long time but, like potatoes, the shape does not permit uniform transfer of heat across the eyelid.
Technology has helped produce equipment such as infrared devices and intense light pulse instruments designed to provide the benefits of the heat compress.
The heat transferred from the warm compress to the eyelid softens the thickened meibum, rendering them easier to express by finger pressure. To maximise the relief from heat compress for MGD, eye lid massage should immediately be performed after the heat compress to restore flow of the lipid secretions so they can contribute to the stability of the tear film. Eyelid massage after heat compress also helps rejuvenate the functions of meibomian glands once the blockages have been eliminated.
Click the link below to get more information about The Dry Eye Handbook
<<<<<<<<DRY EYE REMEDY>>>>>>>>
Or, read further about dry eye below.
MORE INFORMATION
You can get more information about dry eye treatment by clicking on the links below:
- Dry eye remedy and patience
- Dry eye treatment and the most common errors
- dry eye ebook information